Georgia’s Republican governor, Brian Kemp, mentioned that 345,000 individuals would enroll within the state’s Medicaid program, which has strict work necessities—to this point simply 5,118 have.
In 2023, when Georgia launched a Medicaid program that was tied to a strict work requirement, Republican Governor Brian Kemp framed it as a manner to assist individuals get healthcare protection. He made this declare though the state was—and nonetheless is—refusing to increase this system underneath the Reasonably priced Care Act. The brand new plan could be “progressive,” Kemp said, placing “Georgians and their entry to care first.” He mentioned that fifty,000 individuals would be a part of within the first 12 months and that ultimately 345,000 eligible individuals would enroll.
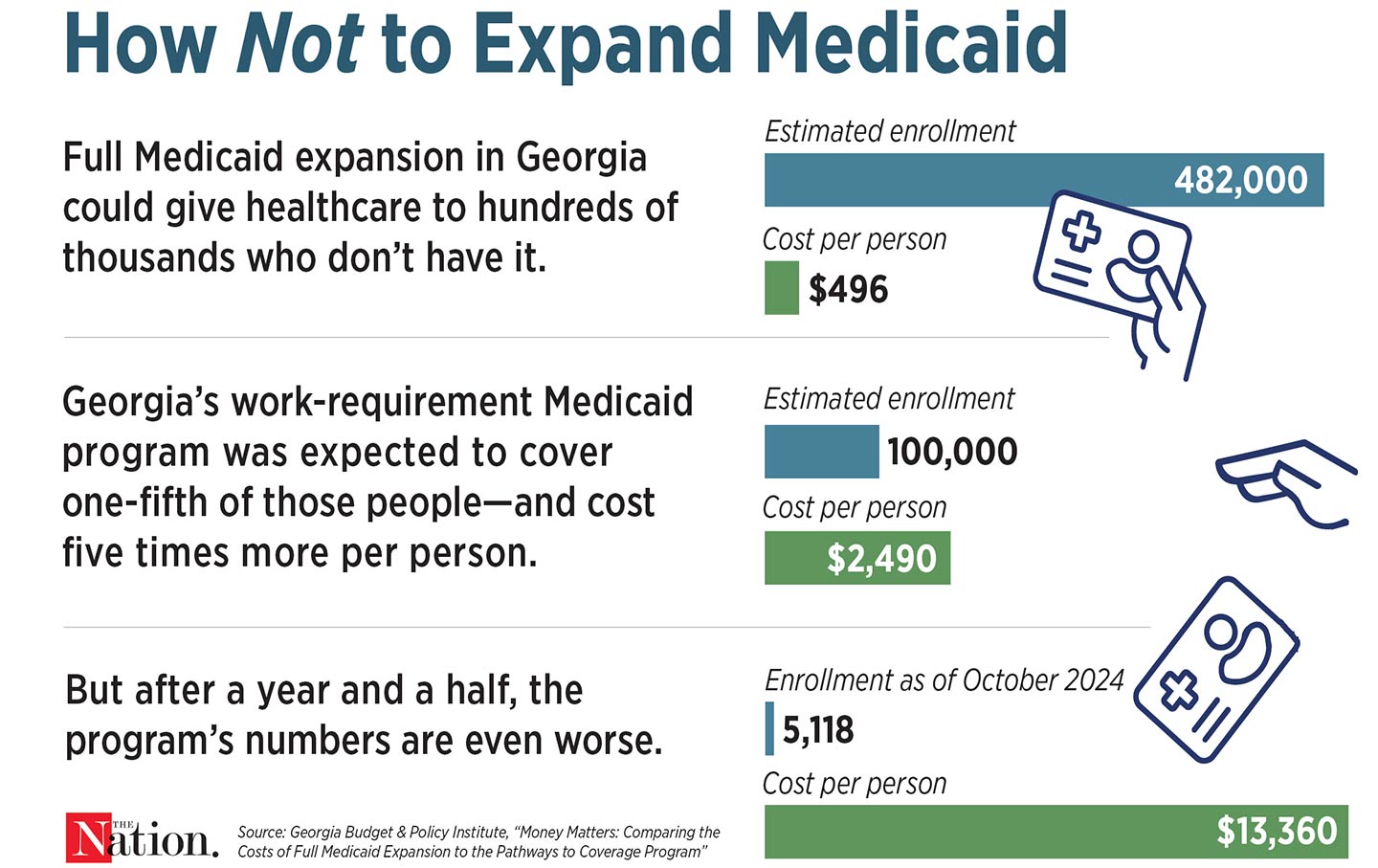
A 12 months and a half later, his guarantees haven’t been borne out: As of the top of October, simply 5,118 individuals were enrolled within the state’s Medicaid work-requirement program—that’s 5 % of the individuals who mentioned they needed to enroll.
A part of the issue is that Georgia’s work requirement is especially harsh. As in different states which have proposed forcing Medicaid recipients to show that they work, individuals in Georgia who earn not more than $31,200 for a household of 4 and need to enroll within the new program need to commonly report that they’re both working, going to varsity, attending job coaching, or volunteering at the least 80 hours a month. However in contrast to these of different states, Georgia’s guidelines apply to individuals as previous as 64 in addition to to those that are caring full-time for his or her youngsters or for different family, don’t have transportation, or are coping with drug dependancy. Different states have additionally proposed giving individuals a number of months as a grace interval to meet the necessities earlier than dropping protection; Georgia can yank it after two months.
The state has additionally made it troublesome for individuals to enroll. Georgians must make their manner via “prolonged questionnaires and technical language,” The Atlanta Journal-Structure reported. The instruments to add paperwork are exhausting to make use of; generally the web site simply stops working. In June, 1,459 individuals tried to enroll in this system however couldn’t, as a result of they had been unable to report their work hours to qualify for protection.
For this, the state is spending a fortune. A 12 months after its launch, this system has value practically $58 million, most of which went to administration and consulting charges, not medical bills.
Georgia may have merely expanded Medicaid to all low- and moderate-income residents, which might have value the state much less and gone rather a lot additional towards Kemp’s purported objective of increasing entry to care. Georgia’s common Medicaid program is already one of many stingiest within the nation: Mother and father can enroll provided that they make lower than $10,000 a 12 months for a household of 4, and adults with out youngsters can’t be a part of in any respect. If Georgia had expanded Medicaid, 359,000 individuals would be capable to enroll. It will even be far cheaper: As an alternative of spending $2,490 to enroll every of the anticipated 100,000 individuals within the work-requirement program, the state would pay simply $496 per particular person in totally expanded Medicaid. However in March, state lawmakers defeated a proposal to increase Medicaid.
The excessive value and ineffectiveness of the work-requirement plan shouldn’t have shocked Governor Kemp. In 2018, Arkansas grew to become the primary state to institute a piece requirement for Medicaid enrollees. This system had no discernible impression on employment, and greater than 18,000 individuals misplaced their Medicaid protection as a result of they couldn’t meet the necessities or end the paperwork. It additionally value the state about $26 million. Such packages in different states have had even larger value tags; in 2019, the federal authorities estimated that Kentucky’s work requirement would value the state $272 million.
However even in states which have adopted Medicaid growth and haven’t carried out pointless work necessities, paperwork prevents hundreds of thousands of Individuals from accessing healthcare. Early within the pandemic, Congress handed laws barring states from kicking anybody off throughout the public well being emergency. That resulted in April 2023, and states resumed making individuals commonly show that they’re nonetheless eligible. Greater than 25 million individuals have misplaced their protection since then, nearly 70 percent of these due to procedural or administrative issues.
The pandemic proved that we may merely preserve individuals enrolled in Medicaid, giving them entry to care that lowers medical debt, improves well being, and reduces deaths. Through the public well being emergency, greater than 21 million individuals signed up when paperwork was halted. However the nation stays obsessive about making individuals show that they’re worthy of protection as a substitute of simply serving to them keep wholesome.